Introduction: A New Era in Diabetes Management
Living with diabetes often means a daily dance with glucose levels, a routine that can feel demanding and, at times, painful. For millions worldwide, the persistent need for less invasive and more convenient methods of monitoring is a constant quest. This search is at the heart of a significant technological leap: the emergence of non-invasive wearable glucose monitors for diabetes. These innovative devices represent a major advancement, promising to shift the paradigm of diabetes management from the current reliance on traditional finger-prick methods, which, despite their utility, have limitations that can discourage regular testing due to pain and inconvenience.

The journey of managing diabetes has historically been marked by the necessity of frequent blood sampling. While effective, these methods often lead to discomfort, potential for infection, and a psychological barrier to consistent self-monitoring. This is precisely where the promise of truly non-invasive glucose monitoring solutions shines. The advancements we’re seeing aim to alleviate these burdens, making the daily task of glucose tracking not just easier, but also more integrated into the fabric of everyday life. Let’s explore the exciting progress in this field and what it means for the future of diabetes care.
The development of these new technologies is a beacon of hope, signaling a future where managing diabetes is less about invasive procedures and more about seamless, data-driven insights. This exploration will set the stage for understanding how these groundbreaking innovations are poised to make life significantly easier for individuals living with diabetes, offering a less burdensome path to maintaining optimal health.
The Journey of Glucose Monitoring: From Pricks to Pixels
The evolution of glucose monitoring devices paints a compelling picture of technological progression, driven by the enduring need for better diabetes management tools. The journey began with traditional blood glucose meters, devices that have been the cornerstone of self-monitoring for decades. These meters require a simple yet definitive action: a finger prick. A small drop of blood is obtained, typically from the fingertip, and then applied to a test strip inserted into the meter. The device analyzes this blood sample to provide a glucose reading, offering a snapshot of blood sugar levels at a specific moment in time.

While instrumental in empowering individuals with diabetes to make informed decisions about their diet, exercise, and medication, these traditional methods come with inherent limitations. The repeated nature of finger pricks can lead to pain, soreness, and calluses. This discomfort, coupled with the occasional inconvenience of needing supplies like lancets and test strips, can sometimes deter individuals from testing as frequently as recommended, potentially impacting the effectiveness of their diabetes management plan.
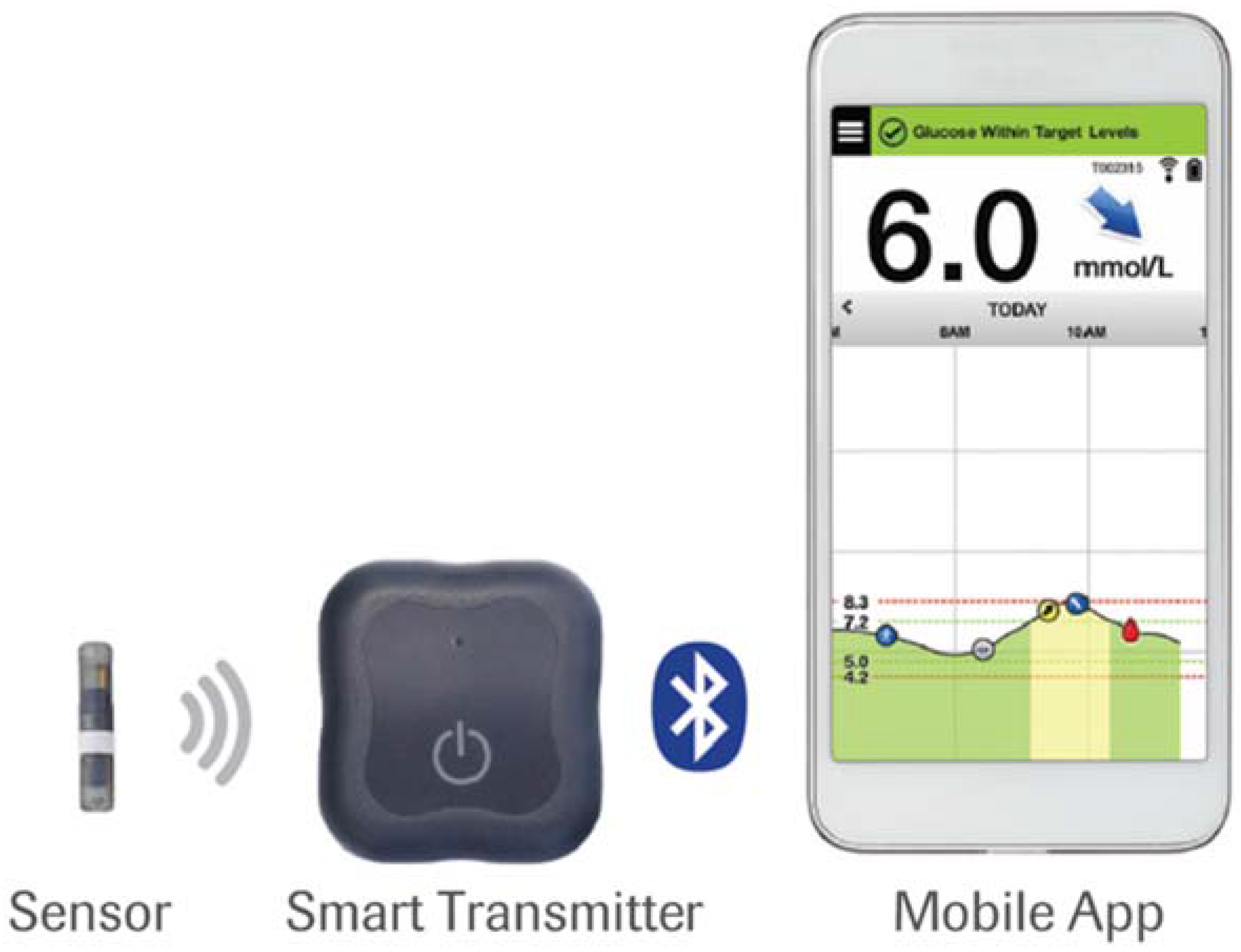
A significant leap forward in glucose monitoring arrived with the introduction of Continuous Glucose Monitors (CGMs). These devices marked a paradigm shift by offering near-continuous tracking of glucose levels. CGMs typically consist of a small sensor inserted just under the skin, usually on the arm or abdomen, which measures glucose in the interstitial fluid. This sensor is connected to a transmitter that sends data wirelessly to a receiver or smartphone app.

The advent of CGMs provided invaluable insights into glucose trends, revealing patterns and fluctuations that a single finger-prick test could easily miss. This continuous data stream empowers users and their healthcare providers to make more timely and precise adjustments to their treatment plans. However, it is important to acknowledge that even current CGMs are considered minimally invasive. The insertion of the sensor, though small, can still cause some discomfort or skin irritation for certain individuals, especially with prolonged use. This mild invasiveness, coupled with the need for sensor replacement, continues to highlight the demand for solutions that eliminate skin penetration entirely. The journey from simple pricks to the sophisticated data streams of CGMs has been remarkable, but the ultimate goal remains a truly painless and effortless way to monitor glucose.
Understanding Non-Invasive Wearable Glucose Monitors
At its core, the term “non-invasive” in the context of glucose monitoring signifies a revolutionary approach: the ability to measure glucose levels without any form of skin penetration. This means no finger pricks, no subcutaneous sensors, and no breaking of the skin barrier. The goal is to achieve accurate glucose readings through methods that are completely painless and unobtrusive.
The ingenuity behind these devices lies in their diverse methodologies for analyzing biological signals. Instead of blood, they focus on other bodily indicators that correlate with glucose levels. This can include:
- Breath Analysis: Certain volatile compounds in breath can be indicative of glucose metabolism. Devices like PreEvnt’s isaac utilize this principle.
- Sweat Analysis: Glucose can also be present in sweat, and researchers are developing sensors capable of detecting these levels.
- Optical Sensing: Technologies such as near-infrared (NIR) spectroscopy analyze how light interacts with skin tissue to estimate glucose concentrations. Devices employing this method, like Apollon’s MOGLU and miniaturized NIR spectrometers, aim for pain-free, optical measurement.
- Interstitial Fluid Analysis: While some methods may indirectly analyze fluid components without full penetration, the truly non-invasive goal is to bypass this altogether.
The primary appeal and ultimate goal of non-invasive wearable glucose monitors are clear: to provide a pain-free, highly convenient, and potentially continuous method for monitoring blood glucose. This offers individuals living with diabetes a significantly less burdensome way to manage their health proactively. The ability to check glucose levels as easily as glancing at a watch, without any physical discomfort or risk of infection, is a game-changer. This directly addresses the core search intent for information on these devices, highlighting their potential to improve adherence and overall quality of life. The vision is to make glucose monitoring so seamless that it becomes an integrated, almost invisible, part of daily living.
The Latest Advancements in CGM Technology and Beyond
The field of glucose monitoring is in constant flux, with the latest advancements in CGM technology pushing the boundaries of what’s possible, moving ever closer to the ideal of non-invasiveness and dramatically enhancing user convenience. While fully non-invasive solutions are still on the horizon for widespread adoption, current innovations are paving the way with novel approaches and improved user experiences.
Several exciting examples of emerging non-invasive and minimally invasive technologies are capturing attention and demonstrating significant promise:
- Breath Analysis Technology: Devices like PreEvnt’s isaac are pioneering the use of breath analysis for glucose estimation. By analyzing specific compounds in exhaled breath, these devices offer real-time glucose insights and can deliver alerts directly to a companion app, providing a completely external method of monitoring.
- Spectroscopy and Optical Sensing: Apollon’s MOGLU is a notable example that employs spectroscopy technology to detect glucose levels through the skin. This method utilizes optical signals, aiming for a painless user experience. With ongoing clinical trials and efforts towards FDA approval, such technologies represent a significant step towards non-invasive monitoring. The promise of miniaturized near-infrared (NIR) spectrometers for accurate, painless monitoring using optical techniques to estimate glucose levels non-invasively is also a key area of development, as highlighted by research in spectroscopy.

These developments underscore a clear trend: the relentless pursuit of less invasive and more data-rich glucose monitoring. The focus is not just on detecting glucose but on doing so in a way that seamlessly integrates into users’ lives, minimizing discomfort and maximizing actionable insights. The integration of these technologies signifies a move towards a more comprehensive and user-friendly approach to diabetes self-management, aligning with the ongoing innovation in CGM systems.
The Power of AI in Diabetes Management Wearables
The integration of artificial intelligence into diabetes management is rapidly transforming how individuals interact with their health data, particularly through AI-powered diabetes management wearables. These sophisticated systems go beyond simply collecting data; they are designed to interpret it, offering insights and guidance that empower users to take more proactive control of their condition.

At the heart of these AI-powered wearables are advanced algorithms capable of analyzing the vast amounts of data generated by glucose monitoring devices. This data often extends beyond glucose readings alone, frequently incorporating user-provided information such as dietary intake, physical activity levels, sleep patterns, and even stress indicators. By synthesizing these diverse data points, AI can construct a more holistic and personalized understanding of an individual’s metabolic health.
One of the most compelling capabilities of AI in this domain is its predictive power. These algorithms can learn from historical data and real-time inputs to forecast glucose trends, anticipating potential highs and lows with remarkable accuracy. In some instances, AI can even provide these predictions or suggest interventions without requiring direct, continuous sensor input, by inferring likely scenarios based on other logged behaviors. This predictive capacity allows individuals to take preventative measures, such as adjusting food intake or activity, to maintain their glucose levels within the target range.

Furthermore, AI excels at providing personalized recommendations tailored to an individual’s unique physiology and lifestyle. Instead of generic advice, AI-driven systems can offer specific, actionable guidance on meal choices, exercise routines, and timing of insulin or medication, all optimized for the user’s current situation and long-term health goals. This level of personalization is crucial for effective daily management and for developing sustainable, long-term health strategies that improve overall well-being and reduce the burden of living with diabetes. The synergy between AI and wearable technology is a testament to the ongoing innovation aimed at making diabetes management smarter and more intuitive.
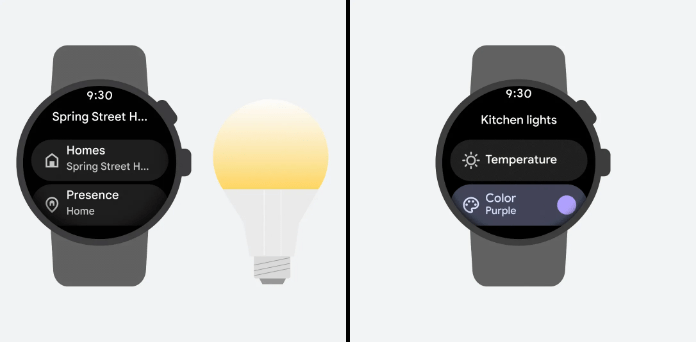
Smartwatches: The Next Frontier for Glucose Monitoring
The prospect of integrating glucose monitoring seamlessly into the devices many of us already wear daily is one of the most exciting frontiers in diabetes technology. The focus on smartwatches with glucose monitoring capabilities represents a significant stride towards making health tracking more convenient and less intrusive for people with diabetes.

The vision is clear: imagine being able to monitor your glucose levels simply by looking at your smartwatch, alongside tracking your heart rate, steps, and sleep. This integration holds the potential to fundamentally change how individuals manage their diabetes by eliminating the need for separate, dedicated devices. While widespread availability is still emerging, numerous manufacturers are actively investing in and developing sensors capable of non-invasive glucose tracking that could eventually be incorporated into popular smartwatch designs. Early reports suggest that breakthroughs are on the horizon, with companies exploring various technological avenues to achieve this goal.
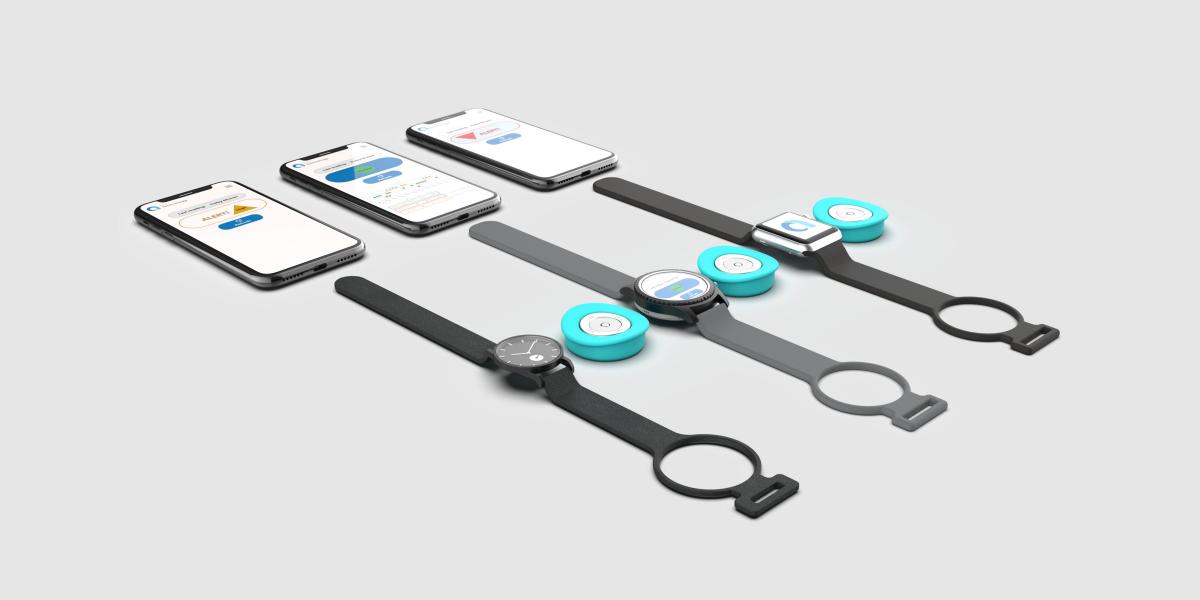
The convenience factor cannot be overstated. For individuals managing diabetes, having a single, stylish device that monitors glucose alongside other vital health metrics would be a remarkable convenience. It means fewer devices to carry, less complexity in daily routines, and a more integrated approach to personal health management. This consolidation not only simplifies the user experience but also encourages more consistent monitoring, as the barrier to checking glucose levels is drastically lowered. The convergence of wearable technology and advanced health sensing in smartwatches promises a future where managing chronic conditions is more accessible, discreet, and integrated into the fabric of daily life.
The Future of Blood Glucose Tracking Devices: A Seamless Vision
Projecting into the future of blood glucose tracking devices, we see a landscape transformed by the convergence of the technologies discussed. The advancements in non-invasive monitoring, CGM innovations, AI integration, and the ubiquity of smartwatches coalesce into a vision of truly seamless, interconnected, and proactive diabetes management.

This future is characterized by wearable solutions that are not only non-invasive but also intelligent and deeply integrated into personal health ecosystems. Imagine a world where managing diabetes is less of a chore and more of an intuitive, data-driven experience. Devices will continuously and painlessly gather glucose data, likely from multiple sources or through advanced optical and biochemical sensing methods, transmitting this information to sophisticated AI platforms. These platforms will then provide highly personalized insights, predictive analytics, and actionable recommendations, all accessible through familiar interfaces like smartphones or smartwatches.

The potential benefits are profound: more precise glucose management leading to better long-term health outcomes, improved patient adherence to treatment plans due to increased comfort and ease of use, and a substantial reduction in the daily burdens and anxieties associated with traditional diabetes management. The ongoing research into technologies like breath analysis, spectroscopy, and advanced sensor development fuels this optimistic outlook. The transition from reactive monitoring to proactive, predictive care is within reach, promising a higher quality of life for millions living with diabetes.
Navigating the Road Ahead: Challenges and Opportunities
While the advancements in non-invasive glucose monitoring are incredibly promising, it is crucial to acknowledge the significant challenges that must be overcome for these technologies to achieve widespread adoption and fulfill their full potential. The path from innovation to everyday clinical practice is often complex and requires addressing several key hurdles.
Key hurdles that need to be navigated include:
- Accuracy and Reliability: Ensuring consistent and reliable accuracy across diverse populations, varying physiological conditions, and different environmental factors is paramount. Non-invasive methods must demonstrate performance comparable to, or exceeding, current standards to gain clinical trust.
- Regulatory Approval: Medical devices, especially those intended for chronic disease management, must undergo rigorous testing and navigate complex regulatory approval processes by bodies like the FDA. This ensures safety and efficacy for patient use.
- Cost and Accessibility: The cost of these advanced devices and their ongoing maintenance needs to be manageable. Furthermore, securing insurance coverage and ensuring accessibility for all individuals with diabetes, regardless of their socioeconomic status, is a critical consideration.
- Data Privacy and Security: As these devices collect sensitive personal health information, maintaining robust health data privacy and security protocols is non-negotiable to protect users from potential breaches and misuse of data.

Despite these challenges, each hurdle presents a significant opportunity for innovation and collaboration within the medtech industry, research institutions, and healthcare providers. Overcoming these obstacles will require dedicated research and development, strategic partnerships, and a commitment to patient-centered design. The drive towards truly non-invasive glucose monitoring is a powerful motivator, pushing the boundaries of science and technology to create a more accessible and effective future for diabetes care.
Embracing the Future of Diabetes Care
The journey we’ve explored highlights a transformative shift in diabetes management, with non-invasive wearable glucose monitors for diabetes leading the charge towards more accessible, comfortable, and proactive self-care. These innovations are not merely incremental improvements; they represent a fundamental reimagining of how individuals can interact with their health, moving from a regimen often dictated by discomfort to one guided by seamless data and predictive insights.

The immense potential of these emerging technologies is multifaceted. From the cutting-edge developments in the latest advancements in CGM technology that continuously refine monitoring, to the intelligent guidance offered by AI-powered diabetes management wearables, and the promise of everyday integration with smartwatches with glucose monitoring capabilities, the collective impact is profound. These advancements are poised to fundamentally change the lives of those managing diabetes, offering greater freedom, reduced burden, and improved health outcomes.

As we look towards the future of blood glucose tracking devices, the vision is one of effortless, integrated, and highly personalized health management. Continued development, rigorous clinical validation, and thoughtful integration into personal health ecosystems will be the cornerstones of realizing this vision. The collaborative efforts of researchers, developers, and healthcare professionals are crucial in navigating the remaining challenges and ensuring these life-changing technologies become a reality for everyone who needs them.

*Stay informed about these rapidly evolving technologies.*
*It is essential for individuals to stay abreast of the latest developments in diabetes care technology. Discussing potential new options and advancements with your healthcare providers is a vital step in identifying the best approach for your individual diabetes management journey. Your healthcare team can provide personalized advice based on your specific needs and circumstances, helping you navigate the exciting landscape of modern diabetes care.*
Frequently Asked Questions
What are non-invasive glucose monitors?
Non-invasive glucose monitors are devices designed to measure blood glucose levels without breaking the skin through methods like finger pricks or sensor insertions. They typically use technologies such as breath analysis, sweat monitoring, or optical sensing (like near-infrared spectroscopy) to estimate glucose concentrations.
When will non-invasive glucose monitors be widely available?
While some devices are in advanced stages of development and clinical trials, widespread availability of truly non-invasive glucose monitors is still emerging. The timeline depends on successful regulatory approvals, technological refinement, and manufacturing scalability. However, significant progress is being made, and availability is expected to increase in the coming years.
How accurate are non-invasive glucose monitors?
The accuracy of non-invasive glucose monitors is a key area of ongoing research and development. While promising results are being reported for various technologies, accuracy needs to be consistently validated across diverse populations and conditions. Regulatory bodies require high levels of accuracy for medical devices, and developers are working diligently to meet these standards.
Can smartwatches monitor blood sugar?
The integration of blood sugar monitoring capabilities into smartwatches is a major focus for many wearable technology companies. While some smartwatches can already track a range of health metrics, non-invasive glucose monitoring is an advanced feature that is still under development. As technology progresses, it is highly anticipated that smartwatches will offer this capability seamlessly.
What is the difference between CGM and non-invasive monitoring?
Continuous Glucose Monitors (CGMs) typically measure glucose in interstitial fluid via a small sensor inserted under the skin, making them minimally invasive. Non-invasive glucose monitoring aims to achieve the same goal without any skin penetration, using methods like breath or optical analysis. The key difference is the absence of any physical entry into the body.
“`